RetinaLink is pleased to feature Aaron Nagiel, MD, PhD, Assistant Professor of Ophthalmology, Children’s Hospital Los Angeles affiliated with the USC Roski Eye Institute – Keck School of Medicine, Los Angeles, CA. Children’s Hospital Los Angeles is one of the eight LUXTURNA™ (voretigene neparvovec-rzyl, Spark Therapeutics, Philadelphia, PA) sites in the United States. Dr. Nagiel exclusively treats pediatric patients with retinal conditions such as retinopathy of prematurity (ROP), retinal detachments, retinal vasculopathies, retinal dystrophies, and other disorders.
Dr. Nagiel incorporated ZEISS’ RESCAN® Intraoperative OCT (iOCT) in his operating room at Children’s Hospital approximately six months ago. We discussed his impressions, learning curve and how he successfully integrated this new and innovative technology.
RetinaLink (RL): What is required to properly setup intraoperative OCT like the ZEISS’ RESCAN in your operating room?
Aaron Nagiel, MD, PhD (AN): A skilled assistant or fellow is always helpful to have during surgery; however, I try to utilize the foot pedal to align the image, change the size of the cube, and make sure the OCT image is properly focused. Almost all functions can be controlled by the foot pedal. Any new technology has a learning curve for me and my surgical team. A surgeon’s investment upfront is worthwhile to learn the best way to identify underlying issues in routine surgical cases.
RL: Children’s Hospital Los Angeles is one of the eight sites participating in the gene therapy treatment with LUXTURNA. How does iOCT assist with the subretinal injection?
AN: There are two main OCT capture methods. One is the macular cube capture which allows one to take a raster scan similar to those done in clinic. The other I find useful is the cross-hair
(2-line) capture that can be obtained in real-time during the surgery. When injecting LUXTURNA, “the live capture allows me to see the bleb rising in real time. The cannula tip can also be visualized entering through the small retinotomy site.”
“Intraoperative OCT is especially useful for gene therapy,” according to Dr. Nagiel. He added, “I know that the injection has gone under the neurosensory retina. iOCT provides critical reassurance, “real time feedback” and this additional data increases surgical confidence.”
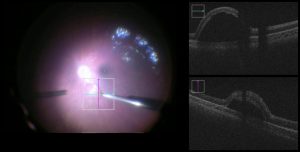
Intraoperative view and simultaneous real-time cross-hair iOCT capture of a subretinal bleb of voretigene neparvovec. (Image copyright: Aaron Nagiel, MD, PhD and Thomas C. Lee, MD)
RL: Are there any limitations with Intraoperative OCT during surgery?
AN: Surgery with the overlay can be distracting at times. Sometimes I will remove the overlay because it interferes with my stereopsis. I’m trying to get more comfortable with it however. Another downside is that the assistant scope does not feature the overlay.
RL: There’s a learning curve to any new technology. How many cases did you do before feeling comfortable with iOCT?
AN: iOCT’s learning curve is reasonable: 5 – 10 cases and I was comfortable. It does require you to work with the foot pedal to become proficient. However, with a retina fellow operating the OCT on the screen it is much easier and good quality images can be acquired almost immediately.
RL: Your colleague calls and asks your opinion of iOCT and mentions it’s too expensive. What’s your response?
AN: There are personal preferences and cost may be an issue at certain facilities. If efficiency is an important metric, then you may feel that taking the time to capture a cube mid-surgery slows you down, even though it only takes a few seconds. At the end of the day, it’s about how much you appreciate having the intraoperative OCT feedback.
RL: A whimisical question… Where do you like to travel when you have some free time?
AN: We have small children so we don’t travel far. A quick trip to Hawaii is always a treat.
Overall, I believe intraoperative OCT has a place in the surgical suite and it’s an asset in my operating room. I believe that leaders in this field such as Justis Ehlers, MD are doing a great job identifying its utility in a variety of surgical situations, and it will eventually become standard on operating microscopes.
Dr. Aaron Nagiel can be reached via e-mail – anagiel@chla.usc.edu

